Is IV Sedation Safe? What Every Dentist Needs to Know About Modern Sedation Protocols
"Is IV sedation safe?" This question comes up in every consultation I have with dentists considering sedation training. It's also the question that stops many qualified practitioners from adding this valuable service to their practice.
The concern is understandable. As dentists, we're trained to "first, do no harm," and any procedure that involves medications affecting consciousness naturally raises safety questions. But here's what might surprise you: modern IV sedation, when properly administered by trained dentists, has an exceptional safety profile that rivals or exceeds many routine dental procedures.
After safely administering over 60,000 IV sedations and training more than 1,000 dentists in proper protocols, I can tell you that the question isn't whether IV sedation can be safe—it's whether you understand the protocols and training that make it safe.
Let's examine the actual safety data, proper protocols, and what every dentist needs to know about administering IV sedation safely and effectively.
The Modern Safety Reality of IV Sedation
Current Safety Statistics
The data on IV sedation safety in dental practice is compelling:
Serious adverse events: Less than 0.1% when proper protocols are followed
Mortality rate: Approximately 1 in 400,000 cases (comparable to local anesthesia)
Patient satisfaction rates: Consistently above 95%
Malpractice claims: Extremely rare for properly trained practitioners
For comparison:
Local anesthesia complications: 1 in 100,000 to 1 in 300,000
Aspirin-related serious events: 1 in 1,000 to 1 in 10,000
Driving fatality risk: 1 in 5,000 annually
The conclusion: When administered by properly trained dentists following established protocols, IV sedation has a safety profile that compares favorably to many everyday activities and medical procedures.
Evolution of Sedation Safety
Historical Context: The safety concerns about dental sedation largely stem from incidents in the 1980s and 1990s when:
Training standards were inconsistent
Monitoring equipment was primitive
Emergency protocols were underdeveloped
Drug selection was less refined
Modern Advances: Today's IV sedation practice benefits from:
Standardized training protocols based on decades of research
Advanced monitoring technology providing real-time vital sign data
Refined pharmacology with predictable, reversible medications
Comprehensive emergency protocols and rescue techniques
Understanding Sedation Levels and Safety
The Sedation Continuum
Minimal Sedation (Anxiolysis):
Patient state: Relaxed but fully responsive
Safety profile: Extremely safe, minimal monitoring required
Examples: Nitrous oxide, low-dose oral medications
Moderate Sedation (Conscious Sedation):
Patient state: Depressed consciousness, responds to verbal/tactile stimuli
Safety profile: Very safe with proper training and monitoring
Examples: IV midazolam, propofol combinations
This is the level most general dentists are trained to provide
Deep Sedation:
Patient state: Depressed consciousness, may not respond to verbal stimuli
Safety profile: Requires advanced training and capabilities
Usually limited to: Oral surgeons, anesthesiologists
General Anesthesia:
Patient state: Unconscious, no response to stimuli
Safety profile: Requires anesthesia training and hospital-level monitoring
Limited to: Anesthesiologists, some oral surgeons
Why Moderate Sedation is Optimal for General Practice
Moderate IV sedation provides the ideal balance:
Sufficient depth for anxious patient comfort
Maintained reflexes including airway protection
Predictable recovery with minimal complications
Reversible effects with available antagonist medications
Essential Safety Protocols for IV Sedation
Pre-Sedation Assessment Protocol
Comprehensive Medical History: ✅ Current medications and potential interactions ✅ Allergies to medications, especially anesthetics ✅ Previous sedation/anesthesia experiences ✅ Medical conditions affecting sedation risk ✅ Social history including alcohol/drug use
Physical Assessment: ✅ Vital signs baseline (BP, HR, RR, O2 sat) ✅ Airway evaluation (Mallampati score, neck mobility) ✅ Heart and lung examination ✅ Weight for accurate drug dosing ✅ ASA classification for risk stratification
ASA Classifications for Sedation:
ASA I: Healthy patients - Ideal candidates
ASA II: Mild systemic disease - Acceptable with precautions
ASA III: Severe systemic disease - Requires careful evaluation
ASA IV: Life-threatening disease - Generally contraindicated
Patient Selection Guidelines
Ideal Candidates for IV Sedation:
ASA I or stable ASA II patients
Ages 16-70 (with experience, can expand range)
Dental anxiety or phobia
Complex procedures requiring patient cooperation
Multiple procedures in single appointment
Relative Contraindications:
Pregnancy (especially first trimester)
Severe sleep apnea
Uncontrolled systemic disease
History of adverse reactions to sedative medications
Inability to follow pre-operative instructions
Absolute Contraindications:
ASA IV patients (unstable)
Acute respiratory infection
Severe cardiovascular disease
Known allergy to sedative medications
Lack of appropriate escort/transportation
Fasting Guidelines and Pre-Operative Instructions
Standard Fasting Requirements:
Solid foods: 6 hours minimum
Clear liquids: 2 hours minimum
Medications: Continue as directed (with exceptions)
Compliance verification: Essential for safety
Pre-Operative Patient Instructions: ✅ Escort requirement: Responsible adult for transportation ✅ Loose, comfortable clothing ✅ Remove contact lenses, jewelry ✅ No alcohol 24 hours prior ✅ Take regular medications (unless specifically instructed otherwise)
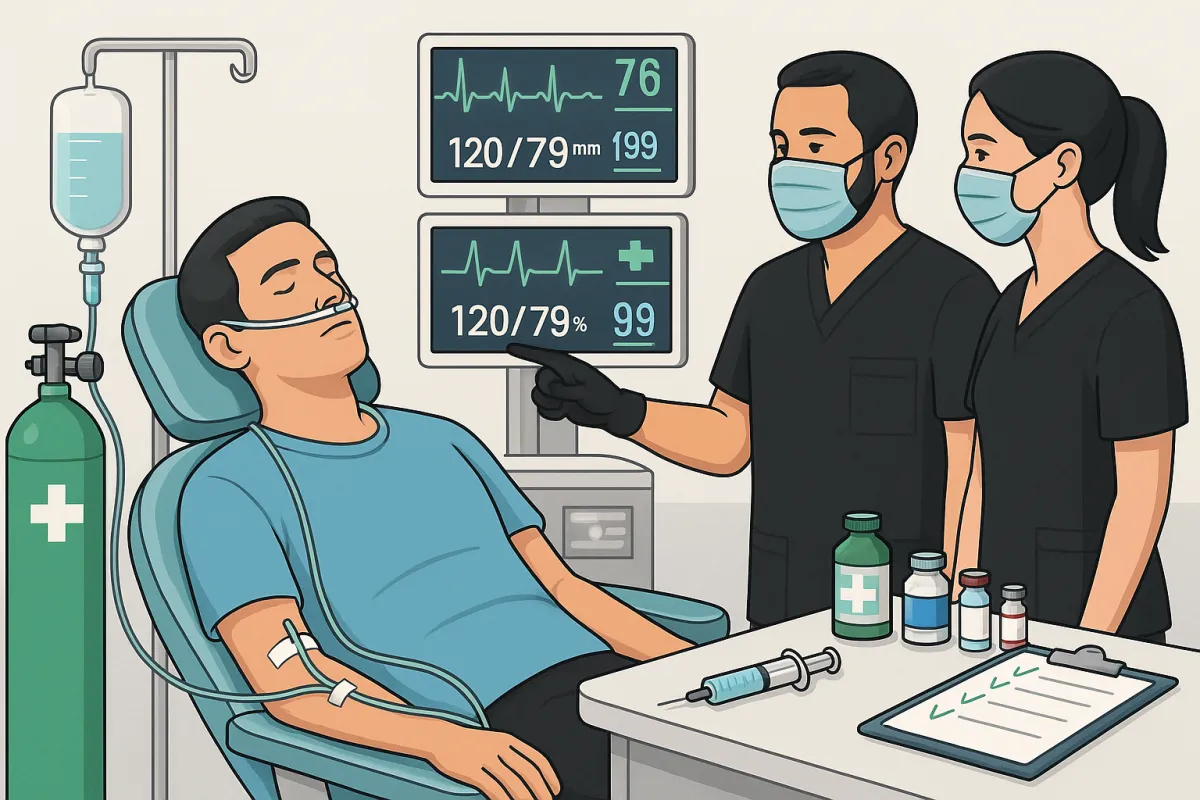
Intra-Operative Monitoring and Safety
Essential Monitoring Equipment
Mandatory Monitoring:
Pulse oximetry: Continuous oxygen saturation monitoring
Blood pressure: Every 5 minutes minimum
Heart rate: Continuous ECG monitoring
Respiratory rate: Visual assessment and monitoring
Level of consciousness: Continuous verbal and physical assessment
Advanced Monitoring (Recommended):
Capnography: End-tidal CO2 monitoring for respiratory status
Pre-cordial stethoscope: Continuous heart and breath sounds
Temperature monitoring: For longer procedures
BIS monitoring: Brain activity assessment (advanced cases)
Medication Protocols and Safety
Primary Sedation Medications:
Midazolam (Versed):
Onset: 1-3 minutes IV
Duration: 30-60 minutes
Advantages: Predictable, reversible with flumazenil
Dosing: 0.02-0.05 mg/kg IV, titrated to effect
Maximum: Typically 5-10mg total dose
Propofol:
Onset: 30-60 seconds IV
Duration: 5-10 minutes
Advantages: Rapid onset/offset, antiemetic properties
Dosing: 0.5-1.0 mg/kg IV, continuous infusion
Caution: Narrow therapeutic window, requires experience
Fentanyl:
Onset: 1-2 minutes IV
Duration: 30-60 minutes
Purpose: Analgesia, reduces sedative requirements
Dosing: 0.5-2 mcg/kg IV
Reversal: Naloxone (Narcan) available
Emergency Medications and Reversal Agents
Essential Emergency Medications:
Flumazenil (Romazicon):
Purpose: Benzodiazepine reversal
Dosing: 0.2mg IV every minute, up to 1mg total
Onset: 1-2 minutes
Duration: 45-90 minutes
Naloxone (Narcan):
Purpose: Opioid reversal
Dosing: 0.04-0.4mg IV, repeat as needed
Onset: 1-2 minutes
Duration: 30-45 minutes
Additional Emergency Drugs:
Epinephrine: Anaphylaxis, severe hypotension
Atropine: Bradycardia, excessive salivation
Succinylcholine: Emergency airway management (advanced training)
Dextrose: Hypoglycemic emergency
Airway Management and Emergency Protocols
Airway Assessment and Management:
Continuous observation of airway patency
Head positioning to maintain airway
Suction availability for secretion management
Oxygen supplementation via nasal cannula
Emergency airway equipment immediately available
Emergency Response Protocol:
Recognition of complication or emergency
Call for help - activate emergency response
Airway management - position, suction, oxygen
Circulation support - IV access, medications
Definitive care - reversal agents, advanced support
Transport if necessary - EMS activation
Common Complications and Management
Minor Complications (1-5% incidence)
Nausea and Vomiting:
Prevention: Avoid overmedication, pre-procedure fasting
Management: Ondansetron 4mg IV, positioning
Recovery: Usually resolves within 30-60 minutes
Excessive Sedation:
Recognition: Reduced responsiveness, respiratory depression
Management: Reduce stimulation, consider reversal agents
Prevention: Careful titration, appropriate dosing
Hypotension:
Causes: Medication effect, vasovagal response
Management: IV fluids, positioning, reduce sedation depth
Prevention: Baseline assessment, gradual titration
Prolonged Recovery:
Causes: Individual variation, drug interactions
Management: Extended monitoring, patient support
Prevention: Appropriate patient selection, conservative dosing
Serious Complications (Less than 0.1% incidence)
Respiratory Depression:
Recognition: Decreased respiratory rate, oxygen desaturation
Management: Airway support, oxygen, reversal agents
Prevention: Appropriate monitoring, conservative dosing
Cardiovascular Events:
Types: Severe hypotension, arrhythmias
Management: Advanced life support protocols
Prevention: Comprehensive pre-operative assessment
Anaphylactic Reactions:
Recognition: Sudden onset, multiple systems affected
Management: Epinephrine, steroids, advanced support
Prevention: Thorough allergy history
Emergency Management Decision Tree
Level 1 Response (Minor complications):
Adjust medication dosing
Provide supportive care
Continue monitoring
Document incident
Level 2 Response (Moderate complications):
Administer reversal agents
Increase monitoring intensity
Consider procedure termination
Prepare for escalation
Level 3 Response (Major emergency):
Activate emergency protocols
Call 911/EMS
Advanced life support measures
Hospital transport if indicated
Training Requirements and Competency
Educational Prerequisites
Minimum Training Standards:
60 hours didactic education covering pharmacology, physiology, monitoring
20 live patient experiences under qualified supervision
ACLS certification (Advanced Cardiovascular Life Support)
Written and practical examinations
Continuing education requirements
Core Curriculum Areas: ✅ Pharmacology: Drug interactions, dosing, metabolism ✅ Physiology: Cardiovascular, respiratory, neurologic effects ✅ Patient assessment: Risk stratification, contraindications ✅ Monitoring: Equipment use, interpretation, troubleshooting ✅ Emergency management: Recognition, response, protocols
Hands-On Clinical Training
Live Patient Experience Requirements:
Supervised cases: Direct instructor oversight
Progressive complexity: Simple to advanced cases
Various patient types: Different ages, medical conditions
Complication management: Simulated and real scenarios
Documentation: Detailed case logs and assessments
Competency Assessment:
Technical skills: IV insertion, monitoring, medication administration
Clinical judgment: Patient selection, dosing decisions
Emergency response: Rapid recognition and appropriate intervention
Communication: Patient interaction, family discussion
Continuing Education and Skill Maintenance
Ongoing Requirements:
State-specific CE hours (typically 8-16 hours every 2 years)
ACLS renewal every 2 years
Equipment maintenance and competency verification
Quality improvement and outcome tracking
Recommended Advanced Training:
Pediatric sedation (if treating children)
Advanced airway management
Difficult patient management
Business aspects of sedation practice
Quality Assurance and Risk Management
Documentation Requirements
Pre-Sedation Documentation:
Complete medical history and physical examination
ASA classification and risk assessment
Informed consent with risks and benefits
Pre-operative instructions and compliance verification
Intra-Operative Records:
Vital signs: Every 5 minutes minimum
Medication administration: Doses, times, routes
Level of consciousness: Continuous assessment
Complications: Any adverse events or management
Post-Operative Documentation:
Recovery progression: Return to baseline
Discharge criteria: Met before patient leaves
Post-operative instructions: Written and verbal
Follow-up plans: Next-day contact, appointments
Facility and Equipment Requirements
Physical Facility Standards:
Adequate space: Room for emergency access and equipment
Lighting: Sufficient for procedures and monitoring
Electrical: Backup power for critical equipment
Oxygen supply: Central or portable systems
Suction: High-volume, reliable suction capability
Equipment Maintenance:
Daily checks: All monitoring and emergency equipment
Calibration: Regular equipment calibration schedules
Backup systems: Redundancy for critical monitoring
Emergency cart: Stocked and checked regularly
Malpractice and Legal Considerations
Insurance Requirements:
Professional liability coverage for sedation procedures
Facility coverage for equipment and premises
Product liability for medications and devices
Coverage limits appropriate for practice size and scope
Legal Compliance:
State board regulations and permit requirements
DEA registration for controlled substances
OSHA compliance for workplace safety
HIPAA compliance for patient privacy
Risk Mitigation Strategies:
Conservative patient selection initially
Comprehensive documentation of all aspects
Regular training updates and skill maintenance
Peer consultation for complex cases
Advanced Safety Considerations
Special Patient Populations
Pediatric Patients (with additional training):
Modified dosing based on weight and development
Enhanced monitoring for smaller patients
Parental consent and involvement
Specialized equipment for pediatric sizes
Geriatric Patients:
Reduced dosing due to decreased metabolism
Increased monitoring for cardiovascular effects
Medication interactions more common
Longer recovery times expected
Medically Compromised Patients:
Cardiopulmonary disease: Enhanced monitoring, reduced dosing
Diabetes: Blood glucose management during sedation
Sleep apnea: Increased respiratory monitoring
Pregnancy: Generally avoided, especially first trimester
Technology Integration and Safety
Electronic Health Records:
Automated alerts for drug interactions and allergies
Standardized protocols built into EHR systems
Quality tracking and outcome measurement
Compliance monitoring for documentation requirements
Advanced Monitoring Systems:
Integrated displays showing all vital parameters
Alarm systems with appropriate limits
Data storage for quality review and legal protection
Remote monitoring capabilities for consultation
Building a Culture of Safety
Team Training and Protocols
Staff Roles and Responsibilities:
Dentist: Primary responsibility for patient care and decisions
Dental assistant: Monitoring support, medication preparation
Additional staff: Emergency response, family communication
Defined roles: Clear expectations and training for each team member
Regular Training Updates:
Monthly team meetings reviewing protocols and cases
Annual emergency drills simulating various scenarios
Equipment training for new devices or updates
Continuing education for all team members
Quality Improvement Programs
Outcome Tracking:
Complication rates: Monitor and trend adverse events
Patient satisfaction: Survey and feedback systems
Efficiency metrics: Recovery times, scheduling optimization
Financial performance: Cost-effectiveness and profitability
Peer Review and Consultation:
Case discussions with experienced practitioners
Difficult case consultation before and during treatment
Professional networks for ongoing learning and support
Mentorship programs for new sedation providers
What Our Graduates Say About Safety
"You can walk out of here and say this is something I can do, I am not worried like I was when I first came in. This course is everything I hoped it would be so that I can get out of here and not be like, 'Wow, this is still too big for me.' And it isn't, they have broken it down so simple, makes it easy, everybody can do it. It is a simple technique and very, very safe. It is fantastic."
- Dr. John Brady, Yuba City, CA
"The key reason [I came] was to learn to incorporate a technique that... has utilized in my office for the past 8 years. To keep it number 1, safe, and just a painless experience for the patient. It is a Course I wish I would have taken 15 years ago. It just delivers a margin of safety that every general dentist with a patient-centered focus worries about."
- Dr. Brent Porter, Santa Cruz, CA
The Western Surgical & Sedation Safety Commitment
Our Safety Track Record
Statistical Excellence:
60,000+ safe sedations administered by Dr. Hendrickson
Zero serious complications in training program history
1,000+ dentists trained with exceptional safety records
100% permit approval rate across all 50 states
Comprehensive Safety Training
Beyond Minimum Requirements:
80+ hours of education (exceeds ADA 60-hour requirement)
2:1 supervision ratio during live patient training
Emergency simulation training with realistic scenarios
Post-training mentorship for ongoing safety support
Unique Safety Features:
Conservative approach emphasizing safety over speed
Real-world experience with thousands of actual cases
Immediate support for questions or concerns post-training
Ongoing education updates on safety advances
Long-Term Safety Support
Graduate Resources:
24/7 consultation line for urgent questions
Annual safety updates and continuing education
Peer network access for case discussions
Equipment and protocol updates as standards evolve
Making the Safety Decision: Your Next Steps
Assessing Your Readiness
Personal Factors:
Commitment to excellence: Safety requires ongoing attention to detail
Willingness to learn: Continuous education and improvement
Conservative approach: Patient safety over convenience or speed
Team support: Staff buy-in and training participation
Practice Factors:
Appropriate patient volume: Sufficient cases to maintain skills
Facility adequacy: Space and equipment for safe practice
Financial commitment: Investment in proper training and equipment
Market need: Patient demand for sedation services
Choosing Quality Training
Essential Training Characteristics:
Exceeds minimum requirements for comprehensive preparation
Experienced instructors with active sedation practice
Live patient experience with appropriate supervision
Emergency training with realistic simulation
Ongoing support for post-training questions
Warning Signs to Avoid:
Promises of "easy money" without emphasis on safety
Minimal hands-on experience or inadequate supervision
Lack of emergency training or protocol development
No post-training support for implementation questions
Conclusion: Safety Through Excellence
The question "Is IV sedation safe?" has a clear answer: Yes, when proper protocols are followed by properly trained practitioners.
The safety of IV sedation isn't a matter of luck or natural talent—it's a matter of:
Comprehensive training that prepares you for both routine and emergency situations
Proper patient selection using established criteria and assessment protocols
Appropriate monitoring with quality equipment and trained staff
Conservative approach that prioritizes safety over speed or convenience
Ongoing education to maintain skills and stay current with advances
The data is overwhelming:
Less than 0.1% serious complication rate with proper protocols
Over 95% patient satisfaction in properly managed programs
Safety profile comparable to local anesthesia when properly administered
1,000+ Western Surgical graduates practicing safely across the United States
But perhaps most importantly: The safety question shouldn't prevent you from providing this valuable service to your patients. Patient anxiety and dental phobia represent real health risks—delayed treatment, avoided care, and compromised oral health create far greater dangers than properly administered IV sedation.
Your patients need safe, comfortable dental care. You can provide it safely with proper training.
The question isn't whether IV sedation can be safe—it's whether you're ready to commit to the excellence that makes it safe.
Start Your Safe Sedation Journey
Book a Free Consultation with Dr. Heath Hendrickson to discuss:
Safety protocols and training standards
Your specific practice situation and readiness assessment
Equipment requirements and facility considerations
Training program details and ongoing support
Questions about patient selection and risk management
Book Your Free Consultation Now →
Dr. Heath Hendrickson has safely administered over 60,000 IV sedations and trained more than 1,000 dentists in safe sedation protocols. His comprehensive training program emphasizes safety excellence and includes ongoing support for graduate success. Learn more about our safety-focused approach at westernsurgicalandsedation.com.
Quick Sedation Safety Facts
✅ Modern IV sedation safety profile:
Less than 0.1% serious complication rate with proper protocols
Patient satisfaction consistently above 95%
Safety comparable to local anesthesia when properly administered
✅ What makes sedation safe:
Comprehensive training (60+ hours minimum)
Proper patient selection and assessment
Real-time monitoring with quality equipment
Emergency protocols and reversal agents available
Conservative dosing and titration approaches
✅ Training requirements for safety:
Live patient experience under expert supervision
Current ACLS certification
Emergency management and airway training
Ongoing continuing education requirements
State permit and facility compliance
Related Resources:



Facebook
Youtube
Instagram